Welcome to Folliculogenesis Part 3!
This is the final installment of a three part series all about ovarian follicles. For a fun visual learning experience I recommend watching my 4 minute video above.
After watching/reading you will learn about:
Two major phases of follicle growth
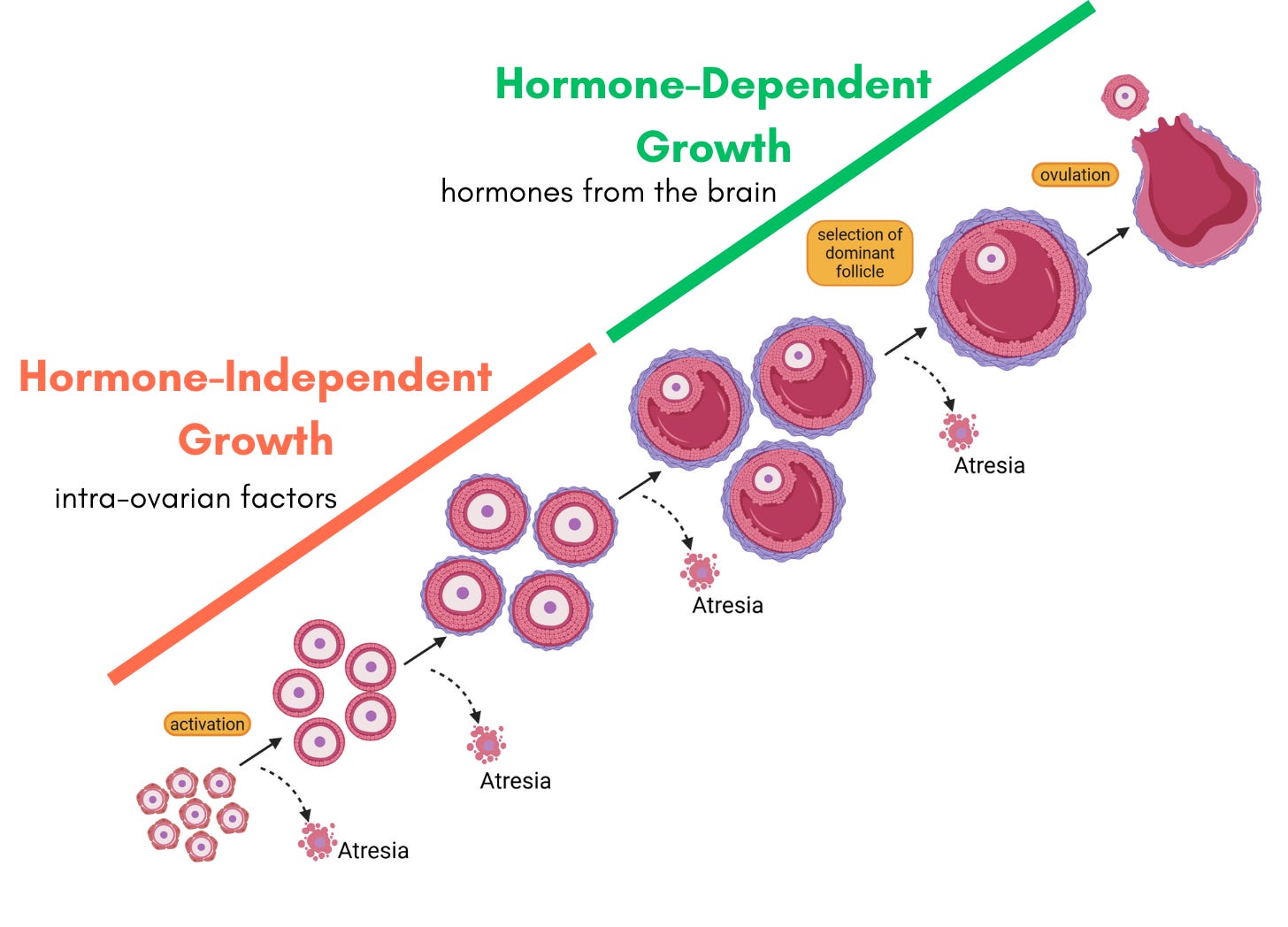
In Folliculogenesis Part 2 we learned about how cohorts of primordial follicles activate and begin follicle growth where along the way many follicles will undergo atresia - or programmed cell death. Eventually, only one dominant follicle is selected to ovulate. During this process, there are two major phases of follicle growth: hormone-independent and hormone-dependent growth.
The first stage when dormant primordial follicles activate and begin growing is the hormone-independent phase. It is controlled by intra-ovarian factors and follicle-to-follicle signaling. Then, once follicles get to a certain size, they rely on hormone signaling from the brain to continue growing - thus the hormone-dependent growth phase.
FSH and LH and the Brain-Ovary Axis
There are two major hormones that follicles need to grow and develop and both are produced in the brain. Follicle Stimulating Hormone (FSH) is involved in follicle growth and Luteinizing Hormone (LH) is involved in ovulation. The brain-ovary axis is the mechanism by which hormones from the brain interact with the ovaries and vice-versa. During the hormone-dependent growth phase of folliculogenesis, FSH is released from the brain and binds to receptors in follicles causing them to grow and produce estrogen. Estrogen in turn feeds back to the brain signaling that it received the message for follicles to grow. This cycle continues as follicles grow, so more FSH is released from the brain and the follicles in the ovary get larger and produce even more estrogen.
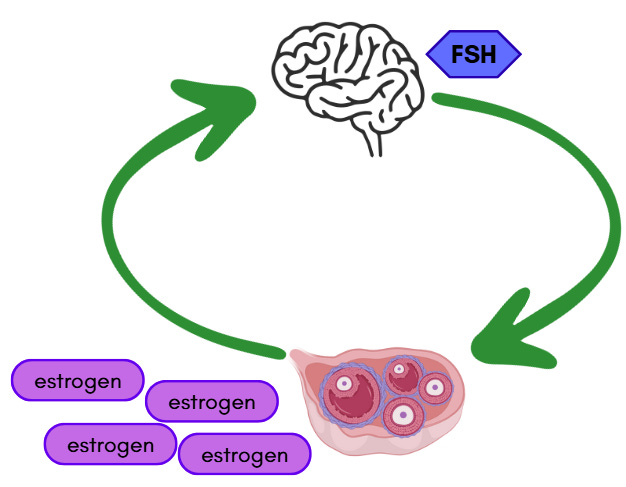
FSH and estrogen are involved in a negative feedback loop which you can think of like a see-saw. As more estrogen gets produced this signals the brain to stop producing FSH and the less estrogen feeding back to the brain, the more FSH production there will be. Eventually, the dominant follicle is producing so much estrogen that FSH production is ceased. Now it is time for ovulation.
The significant increase in estrogen levels signals the brain to release LH which triggers ovulation. The egg, surrounded by a specialized layer of granulosa cells called cumulus cells, is released into the fallopian tube.
What happens to the follicle after ovulation?
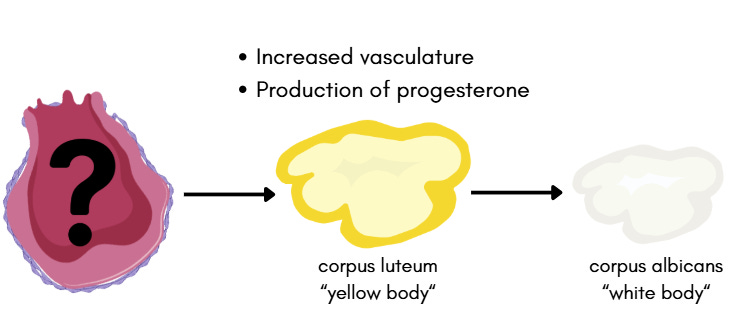
Following ovulation, the granulosa and theca cells from the remnant follicle form what’s called the corpus luteum. In Latin this means yellow body - this structure is yellow because of the lipids it contains. The cells puff up and become increasingly vascularized and produce lots of progesterone. The corpus luteum is critical if the egg that was ovulated is fertilized by a sperm because the progesterone it produces supports the growing embryo until the placenta can take over. If no fertilization occurs, or after the placenta takes over, this structure eventually regresses and forms a white scar called the corpus albicans or white body.
Full follicle life cycle
So bringing the full life cycle of the follicle all together with everything we know we get the following schematic. From dormant primordial follicle all the way to corpus albicans - what a journey!
Next time…
I really hope you enjoyed learning all about follicles in this 3 part series. Next time we will connect everything together and learn about the menstrual cycle.
If you want notifications on new posts please subscribe - it’s free! Free subscribers will also receive a visual infographic they can download about this week’s topic.
References
Schematics and illustrations created with BioRender.com and Canva
Slide 13 H&E image of corpus luteum



















Share this post